The following questions and answers are extracted from Cancer Canada Prostate website. Prostate Edmonton Peer Support Society (PEPSS) has not verified the accuracy of the information offered. PEPSS follow the guidelines set by the Canadian Urology Association. The CUA recommends establishing a PSA benchmark at age 50 or earlier if a family member has been diagnosed with prostate cancer or you are of African heritage.
Under Treatment options, HIFU and Cryotherapy are both offered in Edmonton and the costs are covered by Alberta Health Services.
PEPSS does not offer medical advice or recommendations on any treatment. The Cancer Canada information is presented so each patient understands and makes their own treatment decisions in consultation with their doctors.
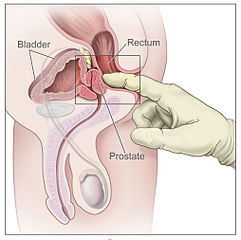
Digital rectal exam (DRE). The doctor inserts a gloved, lubricated finger into the rectum and feels the prostate to check for anything abnormal. It lasts less than a minute, and doesn’t feel much different than a bowel movement. It could save your life, so just do it. Try asking a woman to describe the pelvic exams and mammograms that they have to endure; men have it easy.